As a social worker, it’s critical to have the ability to write detailed and factual social work case notes. Your notes serve as a written record of your client’s symptoms, progress, and treatment decisions and play a crucial role in guiding future interventions and ensuring continuity of care. Studies also show that well-written social work notes can even boost treatment outcomes and speed up progress.
While documenting case notes can be mandatory for billing or maintaining records for insurance audits, it’s also a vital aspect of your being a social worker. Effective note-taking helps you document essential information about your clients, track their progress and interventions, and maintain accurate records for legal and ethical reasons. It also enables you to collaborate better with your team and provide evidence-based services to your clients.
In this article, we’ll delve into some of the best practices for note-taking that are specifically tailored to social workers, along with a practical case notes template for social workers that you can adapt in your daily practice.
Social Work Notes Documentation Formats
| Format | Description | Strengths | Limitations |
| SOAP notes for social workers | Organizes into Subjective, Objective, Assessment, and Plan. | Widely used, clear, supports clinical reasoning. | Can be time-consuming if over-detailed. |
| DAP notes in social work | Covers Data, Assessment, and Plan in a concise format. | Straightforward, less repetitive, efficient. | Less detailed than SOAP for complex cases. |
| BIRP notes | Focuses on Behavior, Intervention, Response, and Plan. | Great for documenting progress and interventions; useful in behavioral health. | May not capture full client history or context. |
| Narrative notes | Free-form style allowing detailed descriptions. | Flexible, captures nuances and context. | Can lack structure, harder to review quickly. |
| Checklist templates | Predefined categories to mark and fill in. | Easy to complete, ensures consistency. | May miss unique client details. |
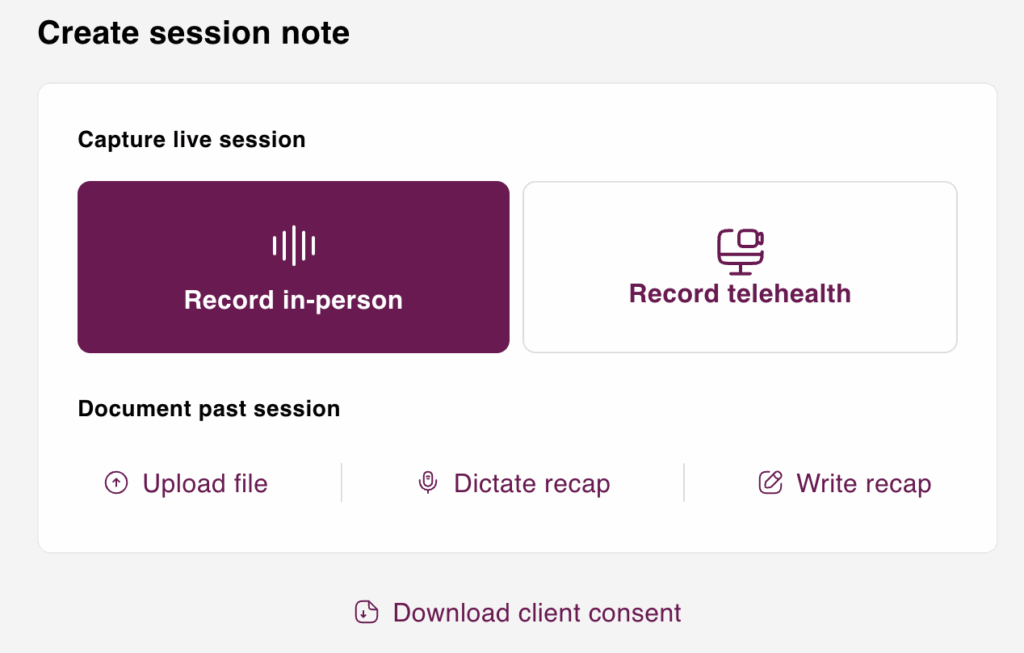
In tools like Mentalyc, you’ll find a wide range of ready-to-use templates designed specifically for social workers—covering everything from crisis interventions and child welfare visits to community mental health sessions and progress notes for ongoing care. Each template is tailored to different client types and therapeutic modalities, so whether you’re documenting a family session, a school-based consultation, or a trauma-focused intervention, you’ll have a structure that fits the situation. Instead of starting from scratch or worrying about missing key details, you can select the right template, adapt it in minutes, and know that your notes meet both professional and compliance standards. This not only saves valuable time but also ensures consistency across cases, freeing you up to focus more on the human connection at the heart of your work.
Why is note-taking in social work so important?
Effective case notes are crucial for social workers for several reasons. Firstly, as you may not work with a particular client forever, they allow for continuity of care. Case notes also help you pass on important information and insights to the next social worker involved in the client’s care. This helps the new social worker understand the specific nuances of the client and suggest ways that have worked for the client in the past. This allows for a smoother transition of care and better outcomes for the client.
In addition to ensuring continuity of care in social work, good case notes also serve as legal documentation of a client’s care. They can be used as evidence in legal proceedings and therefore must be accurate and detailed. Case notes that are incomplete, illegible, or contain subjective opinions can be challenged in court, potentially harming the client’s case.
Finally, good social worker documentation (case notes) also helps social workers to reflect on their practice and improve their skills. By writing down their observations, assessments, and actions taken, social workers can evaluate the effectiveness of their interventions and adjust their approach as needed. This leads to better outcomes for the client and professional growth for the social worker.
An effective way to streamline case notes is by using secure, HIPAA-compliant platforms like Mentalyc. This approach helps therapists save time and reduce documentation stress by providing AI-assisted case notes that are organized, efficient, and tailored to behavioral health documentation standards. Mentalyc allows for secure storage and access, making it easier to document accurately while keeping sensitive information safe.
Which details should I include in my Social Work Case Notes?
As a social worker, taking thorough case notes is crucial in keeping a record of your interactions with clients, tracking progress, identifying challenges, and planning for the next steps. When creating social work case notes, it is important to include key elements such as the name and designation of the person submitting the case note, the services provided during the session, the location and date of the service, and the purpose of the interaction.
Aside from these key elements, other pieces of information to include in case notes are the topics discussed during the session, how the session relates to the treatment plan, how treatment plan goals and objectives are being met, interventions and techniques used during the session and their effectiveness, clinical observations along with any facts, theories, or research underpinning an assessment, tracking of client activities, tracking of program or agency monitoring activities, and evidence that both you and the client have discussed their respective legal and ethical responsibilities.
Moreover, case notes should also contain clients’ or patients’ histories, such as their current strengths and challenges, progress or setbacks, and signs and symptoms related to a diagnosis. Lastly, follow-up information such as the next steps, whether or not the next meeting or follow-up with the client was scheduled, the location and time of the next meeting, and roles and responsibilities for both the client and yourself (or another case manager) to prepare for the next meeting should be included. By taking these steps, social workers can create comprehensive records of client interactions (clinical social work documentation), which can be used to provide better care and track progress over time.
Note template for social workers:
It is essential to have a structured approach to note-taking to ensure accuracy, consistency, and confidentiality. Below is a note-taking template for social workers that will help you stay organized and focused while documenting your client interactions.
Social Work Case Note Example:
Date: April 3rd, 2023
Client: Michael Johnson
Case: Substance Abuse
Summary:
Mr. Johnson, a 42-year-old male, sought help for his substance abuse issues during our initial assessment. He reported a long history of alcohol and drug abuse, which he attributed to coping with work-related stress and relationship problems. His substance use has negatively impacted his work performance and relationships, with his partner threatening to leave him if he doesn’t seek help.
I conducted a substance use assessment and provided Mr. Johnson with psychoeducation about the physical and mental health consequences of substance abuse. I also shared information about the various resources available to him, such as support groups and treatment programs.
Mr. Johnson expressed a willingness to seek help and agreed to attend a substance abuse support group in his community. I provided him with the necessary information about the meeting times and location of the support group and encouraged him to attend regularly.
During our session, we also discussed the importance of developing coping skills to manage stress and prevent relapse. I gave him information about mindfulness and relaxation techniques and encouraged him to practice them regularly.
Moving forward, I will continue to work with Mr. Johnson to monitor his progress and provide support as needed. Additionally, I made a referral to a local treatment program and will follow up with Mr. Johnson to ensure that he receives the care he needs.
What are some practical tips for Writing Effective Social Work Notes?
Effective case notes provide a comprehensive and accurate record of a client’s history, treatment, and progress and are essential for ensuring continuity of care and collaboration among healthcare providers.
Here are some key characteristics that make social work notes effective:
Use a standard format for Social Work Progress Notes
Using a standard format for your notes can help ensure that you are documenting all the necessary information and make it easier to share information with other team members. Many organizations have their own standard format for documentation, but if yours does not, consider creating your own template. Include sections for client demographics, history, presenting problem, treatment plan, progress, and any relevant information related to legal or ethical concerns.
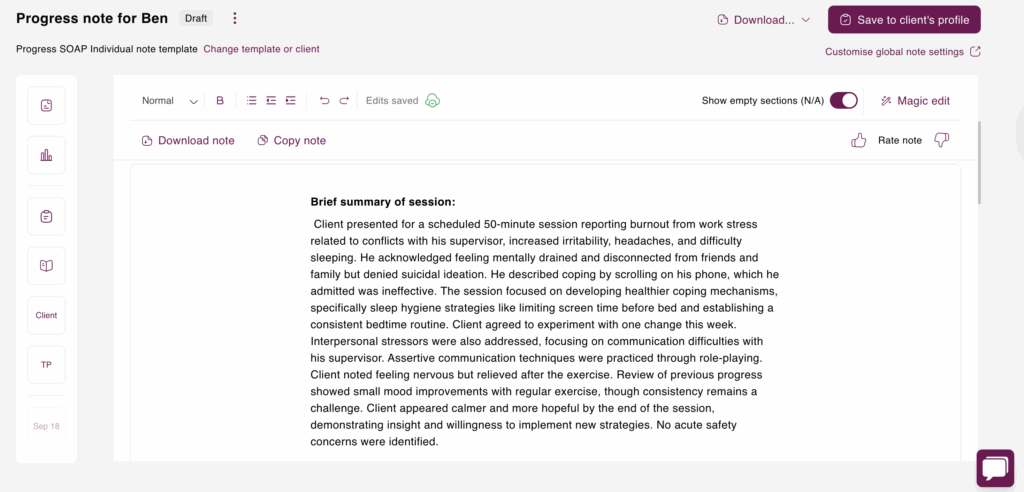
Here’s an example of a SOAP note generated by Mentalyc:
Subjective:
The client presented for a scheduled 50-minute session reporting burnout stemming from work-related stress, particularly conflicts with his supervisor. He described this stress as manifesting in increased irritability, headaches, and difficulty sleeping, averaging only 4-5 hours per night. Furthermore, he reported feeling mentally drained and disconnected from friends and family, though he denied any suicidal ideation. He identified scrolling on his phone as his primary coping mechanism, acknowledging its ineffectiveness. He also alluded to past family dynamics contributing to feelings of inadequacy, but these were not explored in detail during this session.
Objective:
The clinical interview served to assess the client’s presenting concerns, explore contributing factors, and identify appropriate interventions. No acute safety concerns were identified, as the client denied suicidal or homicidal ideation. Assertive communication techniques were practiced through role-playing, after which the client reported feeling nervous but relieved. A review of previous progress indicated slight mood improvements correlated with regular exercise, although maintaining consistency with exercise remains a challenge.
Assessment:
The client demonstrated engagement and openness throughout the session, actively participating in discussions and exercises. He expressed a willingness to explore his challenges and implement new strategies, indicating a positive therapeutic alliance. His willingness to experiment with a small change this week suggests a promising initial response to the interventions discussed.
Plan:
The plan is to continue weekly sessions focused on building coping skills, improving sleep, and practicing assertive communication. For homework, the client agreed to experiment with one small change this week, such as incorporating a calming activity before bed, like listening to music. Continued treatment will involve ongoing weekly sessions to reinforce these skills and monitor progress.
Stay neutral in Social Work Documentation
It is important to maintain objectivity in your observations when writing case notes. While it is impossible to completely eliminate your own subjective lens, you can strive to be more aware of it. When writing your observations, focus on providing descriptive details rather than subjective interpretations. For instance, consider the following two examples:
Example 1: The client angrily stated, “Get out of my house!”
Example 2: The client spoke in a loud voice, saying, “Get out of my house!”
In the first example, the social worker has added their own perception that the client was angry. However, this interpretation may not be entirely accurate and could affect future interactions between the client and other social workers. By simply stating that the client spoke in a loud voice, the observation becomes more objective and less judgmental. This practice is especially helpful when documenting client progress effectively so that future interventions are based on facts rather than assumptions.
Use chronological order
When writing case notes in social work, it is important to resist the urge to group incidents together thematically and instead present them chronologically. As humans, we naturally have a bias toward stories and tend to weave seemingly unrelated events together to form a coherent narrative.
However, when it comes to documenting our interactions with clients, it is important to write down things as they happened, in the order they occurred, rather than how we perceived them to have happened. By presenting a blow-by-blow account of our interactions with clients, we avoid distorting reality and placing our own subjective lens on what happened.
Platforms like Mentalyc can support this by helping you structure notes chronologically, making it easier to organize events clearly without losing essential details. This not only maintains the integrity of case records but also helps present client information objectively and securely.
Mentalyc AI Note-Taking App Pricing & Plans
| Plan | Price | Key Features |
| 14-Day Free Trial | $0 | 14 days of full PROaccess, including 15notes—no credit cardrequired. |
| Mini | USD 14.99 /month | Record in-personsessions, upload audiofiles, use voice-to-text,or type notes directly, etc |
| Basic | USD 29.99 /month | Everything in Mini, plus:Alliance Genie™ NEW!(limited access), Smart TP™ |
| Pro | USD 59.99 /month | EMDR, Play andPsychiatry modalities,100+ custom templatesincld. BIRP, PIRP,GIRP, PIE, and SIRP,Auto-computed CPTcodes |
| Super | USD 99.99 /month | Everything in Pro, plus:Group therapy notes foreach group member,Priority onboarding andsupport |
For more details, visit the pricing page on our website.
Explain your assessment Clearly in Social Work Notes
Including an explanation of how you arrived at your assessment in your case notes is crucial for ensuring that others can understand and evaluate your conclusions. As a reader, it can be confusing to see an assessment without any context or reasoning behind it.
Be sure to outline what factors informed your assessment. Did you base your conclusions on a particular theory or model? Did you make observations or conduct an interview with the client? Providing this information not only helps others understand your thought process but also helps you stay accountable for your conclusions. It’s important to be transparent about how you arrived at your assessment to ensure the validity and reliability of your case notes. Using structured note-taking templates can also make this process smoother and more consistent across sessions.
Dedicate time in your day
Incorporating case notes into your daily schedule can alleviate the frustration that comes with adding them to an already busy day. Allocate time for reviewing and writing case notes during each session. Try dedicating 10–15 minutes after each session to draft notes while the details are still fresh in your mind. This will ensure accuracy and allow you to reflect on the session or make notes for the next one.
Make sure to set aside 10-15 minutes before each session to go over notes from previous sessions. This will help you not miss important details, which can improve your relationship with clients and treatment suggestions. Checking notes can also assist in directing the session, making sure you and your client stay on track with treatment goals.
Be objective and concise
Your notes should be factual and objective, avoiding any personal biases or opinions. Stick to the facts and document what you observe and hear from the client. Avoid using emotional language or making assumptions about the client’s situation. Following social work note-taking best practices, your notes should also be concise, focusing on the most important information. Use clear and simple language, and avoid using jargon or acronyms that may be confusing to others who read your notes.
Document Social Work Notes regularly and on time
Documenting regularly and in a timely manner is important to ensure that your notes are accurate and up-to-date. Try to document your interactions with clients immediately after the session, while the information is fresh in your mind. If you need to document later, make sure to review any notes or recordings you may have taken to ensure accuracy. Consistent therapy session documentation helps maintain accuracy and continuity across client records.
Focus on client strengths
As a social worker, it’s important to focus on the strengths of your clients, not just their problems. Your notes should reflect this by documenting the client’s strengths, resources, and coping skills. This can help the client feel empowered and motivated to work towards their goals.
Keep confidentiality in mind
Confidentiality is a critical aspect of social work practice, and your notes should reflect this. Make sure to document sensitive information securely and confidentially, following your organization’s policies and procedures for safeguarding client information. Avoid sharing information with others who are not involved in the client’s care, and only share information with other team members on a need-to-know basis. Proper confidentiality and secure storage for client data is essential for ethical practice.
Be aware of legal and ethical considerations in Social Work Documentation
As a social worker, you are bound by ethical and legal standards when it comes to documentation. Your notes should reflect these standards by being accurate, complete, and objective. Make sure to document any legal and ethical considerations in case notes that arise during your interactions with clients, and follow your organization’s policies and procedures for reporting these concerns.
Ensure the security of your Social Work Case Notes
It’s essential to remember that case notes can contain highly sensitive information about your clients, which means they should be kept secure. The HIPAA protects the medical records, such as treatment notes. Maintaining HIPAA-compliant social work notes ensures that these records are both legally protected and ethically managed.
To ensure the highest level of security for your treatment notes, it is best to save them in a cloud storage system that is encrypted and requires a password. When you need to access these notes, avoid using unsecured servers like public networks at coffee shops. Also, be cautious when setting up passwords. Avoid repeating them or sharing them with others, and don’t use easy-to-guess passwords, like your name or date of birth. Additionally, it is important to physically secure the devices where you store your notes, by locking them or using other security measures. To safeguard your notes even further, consider adding a feature that will wipe your device’s memory in the event it gets stolen.
Protect your case notes from third parties
It is crucial to safeguard your case notes from unauthorized access by third parties, who might attempt to obtain them through legal means. The rules governing the release of case notes by social workers in response to a subpoena can differ from one state to another and may hinge on the specific terms of the subpoena. To ensure that your clients’ privacy interests are respected while also preserving their treatment objectives, consider keeping case notes that are brief but informative. Maintaining concise records still allows you to meet behavioral health documentation standards without revealing unnecessary personal details. Rather than providing a detailed account of every aspect of a client’s marital discord, for example, you could simply record that the client had an argument with their spouse, or that it was part of an ongoing pattern.
Ask your supervisor for feedback on your Social Work Notes
Feedback is essential in any profession, and mental health is no exception. Your supervisor can provide valuable insights into the quality of your social work case notes, helping you identify areas where you can improve. By providing constructive criticism, they can help you develop new skills and techniques to enhance your note-taking abilities.
When asking for feedback, be specific in your request. Instead of asking for general feedback, ask your supervisor if there is anything specific you can do to write better case notes. This shows that you are taking the initiative to improve and that you value their expertise and opinion.
Checklist for Effective Social Work Notes
| Criteria | Details |
| Objective and factual documentation | Record only what was observed or stated, avoiding bias or assumptions. |
| Clear structure | Use structured note-taking templates like SOAP or DAP for consistency. |
| Timeliness | Write social work progress notes immediately or soon after the session. |
| Confidentiality and secure storage for client data | Ensure HIPAA compliance, encrypted storage, and restricted access. |
| Legal and ethical considerations in case notes | Follow agency policies and professional standards. |
| Client strengths included | Highlight positive attributes, coping strategies, and resources. |
| Continuity of care | Document progress and follow-up plans to support future interventions. |
| Insurance and billing compliance | Ensure notes meet payer requirements for audits and reimbursements. |
The Bottom Line
Note-taking is an essential part of social work practice. By using a standard format, being objective and succinct, documenting regularly and promptly, focusing on client strengths, keeping confidentiality in mind, and being aware of legal and ethical considerations, you can create accurate and effective notes that support evidence-based services for your clients.
Notes don’t have to drain your time or energy. Mentalyc is designed with social workers in mind. It offers templates for everything you handle – home visits, crisis interventions, family sessions, etc. so you’re never stuck starting from a blank page. With Mentalyc’s ready-made templates, AI-assisted drafting, and HIPAA-secure storage, you can create professional, supervisor- and insurance-ready documentation in minutes. Spend less time buried in paperwork – and more time supporting the clients and communities who need you most.
Here’s how social workers describe the changes Mentalyc has brought to their practice:
Sasha Kendall, LCSW:
“My notes get finished after every single session now, because Mentalyc makes it so easy. I am not stressed out about notes, and I always just feel like I’ve got extra time, and I’m not stressing out, and I feel like my notes are of much higher quality.”
Amber McKinney, LCSW:
“The most helpful feature on the platform is the integration of everything, you name it, from treatment planning and factoring in that treatment planning into diagnosis into the progress note. The platform takes care of what’s called the insurance golden thread. It weaves it all together and gives you everything you need to make sure you have a compliant, well written note.”
Frequently Asked Questions (FAQs) on Social Work Case Notes
Why other mental health professionals love Mentalyc
“It takes me less than 5 minutes to complete notes … it’s a huge time saver, a huge stress reliever.”
Licensed Marriage and Family Therapist

“It’s so quick and easy to do notes now … I used to stay late two hours to finish my notes. Now it’s a breeze.”
Licensed Professional Counselor

“A lot of my clients love the functionality where I can send them a summary of what we addressed during the session, and they find it very helpful and enlightening.”
Therapist

“Having Mentalyc take away some of the work from me has allowed me to be more present when I’m in session with clients … it took a lot of pressure off.”
LPC







