How many times have you stared at your notes thinking, ‘What exactly do I need to include so this is compliant and makes sense later? You may wonder what a progress note should include or what mental health progress note templates to use.
When you are writing therapy progress notes, there isn’t one template that is recommended. Many insurance companies require you to state what interventions you’re using and why the client needs therapy—otherwise known as medical necessity. This is easy when you have well-documented reasons why the client is seeing a mental health professional, and you use sound clinical practices.
If you want to know what common templates or best psychotherapy note formats for your mental health progress notes look like. Here are 15 examples you can use.
1 – SOAP Note Template and Example for Mental Health Progress Notes
A SOAP note template for therapy is a common note format that many mental health professionals use to document their sessions. A SOAP note has four sections, and an example is provided below.
Subjective: The client presents for therapy, wanting to work on symptoms associated with their Borderline Personality Disorder diagnosis. The client reports having trouble with their interpersonal relationships and often feels like the people close to them will abandon them. The client says they struggle to relate to their coworkers and maintain friendships. The client states they have had these problems throughout their life but noticed the relationship difficulties increasing in the last few months.
Objective: The client presents with a disheveled appearance. They are on time for the session and have a depressed presentation. The client appears in a low mood.
Assessment: The client appears to meet the Borderline Personality Disorder criteria. They have a history of challenges with maintaining friendships, which has increased in the last few months with increased stress.
Plan: The client will meet with the therapist weekly to work on symptoms associated with Borderline Personality Disorder. The therapist will utilize DBT techniques, such as helping the client learn interpersonal effectiveness skills. In addition, the therapist will work towards helping the client identify a DBT group in the area they can join.
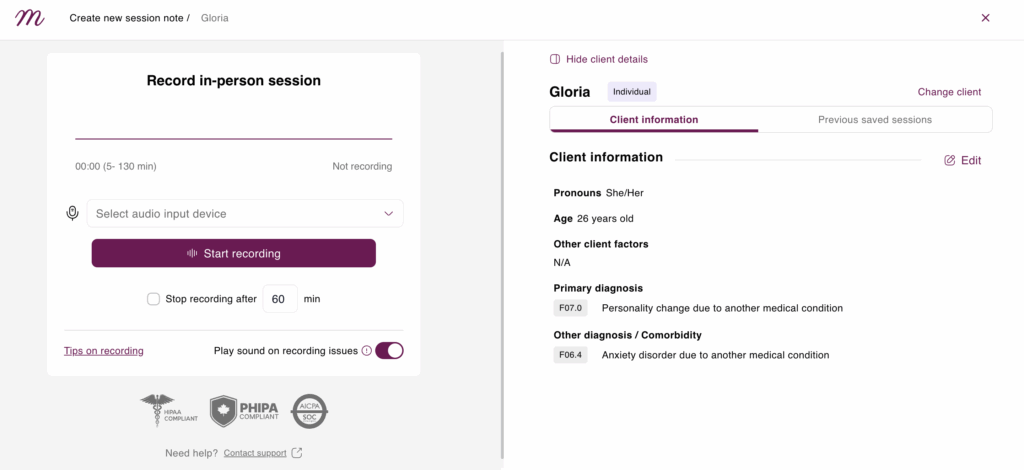
With Mentalyc, documenting sessions with SOAP notes has never been easier. This tool gives you access to ready-to-use SOAP templates (and more) that help you quickly capture session details in a clear and organized way. You can customize the layouts to match your style and workflow, saving time while keeping your documentation consistent, professional, and compliant.
2 – DAP Note Template and Example for Therapy Documentation
DAP notes have three short sections, so it’s easy to track a client’s progress. Here’s an example of a DAP note for a client with ADHD.
Data: The client presents for psychotherapy due to struggling to focus on his college classes. The client finds they procrastinate and need help completing their homework by assigned deadlines. The client has consistently been late in turning in homework since the semester began. He also reports problems getting to class on time since the semester started three months ago.
Assessment: The client’s symptoms are consistent with ADHD. The counsellor will work with him on strategies to help with task initiation as well as recognizing unhelpful thoughts he may be having that inhibit his ability to get his work done. The counsellor will also speak with him about getting a formal assessment done for ADHD and potential medication.
Plan: The client will meet with the counsellor weekly to work on strategies for coping with ADHD. The counsellor will give him an outside referral to a Psychologist who does ADHD testing.
3 – BIRP Note Template and Example for Behavioral Health Progress Notes
BIRP notes are behavior-focused notes that have four sections. An example of a BIRP note template for trauma is provided below.
Behavior: The client presents for therapy to work on challenges related to childhood trauma. The client reports that they are having flashbacks and nightmares regarding a sexual abuse incident that occurred in childhood. Additionally, the client reports that these nightmares have affected their sleep quality, causing fatigue issues during the day.
Intervention: The counsellor will utilize EMDR techniques to help treat the client’s trauma. The counsellor spent the first part of the session identifying coping skills and resources they use to process trauma and what hasn’t helped.
Response: The client was on time for therapy and attentive. The client is receptive to starting EMDR, which will begin in the next session.
Plan: The client and counsellor will start working on the first phase of EMDR in the next session. The counsellor and client will meet weekly to work on the client’s past trauma.
Therapists who frequently use the BIRP notes format can benefit from structured layouts as part of counseling documentation templates to keep their records consistent.
Difference Between SOAP, DAP, and BIRP Notes
| Feature | SOAP Notes | DAP Notes | BIRP Notes |
| Full Form | Subjective, Objective, Assessment, Plan | Data, Assessment, Plan | Behavior, Intervention, Response, Plan |
| Purpose | Detailed, medical-style documentation | Simplified format for mental health | Focuses on behavioral interventions and outcome |
| Best For | Medical & clinical settings | General therapy notes | Behavioral health and intervention tracking |
| Detail Level | High | Moderate | Moderate |
| Used By | Therapists, psychiatrists, clinicians | Therapists, counselors | Behavioral therapists, social workers |
Tools like Mentalyc gives you access to a variety of progress note templates, making it quick and easy to document sessions in a way that fits your needs. Whether you prefer SOAP, DAP, BIRP or other formats you’ll find ready-to-use layouts that make your work easier and keep your documentation consistent. You can also customize them to match your own style and requirements, saving time while maintaining a professional look for your notes.
4 – GIRP Note Template and Example Goal-Oriented Therapy Notes
GIRP notes are goal-focused notes that have four sections. A GIRP note example is provided below.
Goal: The client presents for therapy, wanting to work on several life stressors. The client presents for treatment due to several recent changes they are having trouble adjusting to. The client reports they just got married and started a new job. The changes they’re facing are causing a lot of stress and exhaustion.
Intervention: The counsellor will work with the client on developing 3-5 strategies for reducing and coping with stress. The counsellor will allow the client space to discuss and process how stress impacts them.
Response: The client states they “are happy to start therapy and work on stress management skills.” The client is attentive and focused in the therapy session.
Plan: The counsellor will meet with the client bi-weekly to address stress management techniques. The client’s next session is Friday at 10 a.m.
5 – PIRP Note Template and Example for Problem-Focused Progress Notes
PIRP notes are problem-focused notes that have four sections. An example of a PIRP note is included below. A PIRP note example is included below.
Problem: The client presents for therapy and states her problems include meth use and depression. The client reports, “meth use has ruined my relationships with others.” The client struggles to pay her bills and says she has been clean from methamphetamine for one week. The client would like to work on assistance with paying her bills and identifying additional recovery resources to help her continue abstaining from meth use.
Intervention: The therapist utilized motivational interviewing techniques to assess their substance use history and readiness to change. The therapist helped the client explore triggers for using methamphetamines. The therapist gathered a history of the client’s depressive symptoms, and the client states they have been depressed for about two years when their methamphetamine use increased.
Response: The client appears to be in the action stage of change with their methamphetamine use. The client reports they are motivated to stay clean and learn more about their depression and substance use.
Plan: The client will attend weekly therapy sessions with the therapist. The client will attend one NA group per week. The therapist will refer the client to have services with a caseworker who can help them address assistance resources for paying their bills.
For therapists who’d like to make documentation smoother and more efficient, there are digital tools like Mentalyc that can help simplify note-taking, including SOAP notes and other formats, while still keeping detailed, organized records. Reducing time spent on paperwork can make it easier to stay focused on clinical care—learn more about options here.
6 – Custom Format Mental Health Progress Note Template and Example
This note doesn’t follow a specific template, but includes necessary and relevant information for billing and insurance purposes. Understanding what should be included in a progress note is key for compliance and clarity.
Mental status: The client presents with a euthymic mood. The client appears well-dressed and speaks at an average volume and pace. The client is oriented to person, place, and time.
Risk assessment: The client presents no significant risk of harming themselves or others.
Presenting Problem: The therapist and client have been working to address problems in communication in their relationships with their partner and friends. They are working on using “I” statements.
Assessment: The client reports difficulty in their relationships before engaging in therapy. The therapist has been educating the client about healthy relationships in prior sessions. The client says that they have been able to utilize “I statements” when bringing up difficult conversations with their partner.
Therapist intervention: The therapist has provided the client with psychoeducation on healthy communication skills and introduced them to Gottman’s Four Horsemen of the Apocalypse.
Plan: The client is progressing in therapy and will probably need two more sessions to complete their work. The client will meet with the therapist next week and the following week and then terminate treatment at this time.
Progress notes aren’t just paperwork – they should tell the unique story of each client. That’s why it’s great when you can choose the note format that works best for both you and your client. With Mentalyc, you can make them faster, easier, and more consistent than ever.
7 – Case Management Note Template and Example
Case workers or case managers may work on areas related to a client’s mental health, but their focus is a little different from that of a typical mental health clinician. This case management note template provides a useful structure for professionals handling clinical case management.
Problem: The client presents for case management services to work on finding housing and applying for food stamps. The client reports that they were able to obtain the paperwork on their own but need help filling it out. The client has been staying in a homeless shelter, and would like to find their own place.
Treatment plan goal: The client will obtain housing and food assistance.
Intervention: In this session, the case manager was able to spend an hour assisting the client with filling out applications for food stamps and low-income housing. The case manager educated the client on where to turn in filled out applications and provided them with transportation to the community service agency.
Client response: The client filled out their applications and expressed gratitude for the assistance of the case manager.
Plan: The case manager will meet with the client bi-weekly to help the client track the progress of their applications and if denied help them access other community resources.
8 – CBT Note Template and Example Using SOAP Format
CBT (Cognitive Behavioral Therapy) notes can use other note formats to document the therapy session. In this example, there are CBT interventions using a SOAP note format.
Subjective: The client presents for therapy due to social anxiety. The client states they don’t like leaving their house because they don’t want to interact with people they don’t know. In addition, they often have to lead meetings and give presentations at work, making them feel jittery. The client reports poor sleep quality and work difficulties due to social anxiety.
Objective: The client has an anxious presentation. They are talking rapidly during the session. The client appears nervous and anxious while speaking with the psychotherapist.
Assessment: The client has symptoms consistent with social anxiety disorder. The psychotherapist will monitor their anxiety symptoms through the Liebowitz Social Anxiety Scale. The psychotherapist will work with the client utilizing CBT methods to identify and replace irrational thoughts. The psychotherapist will also work with the client to help them identify cognitive distortions and how these distortions may effect their life.
Plan: The psychotherapist and client will meet weekly for therapy. The client will keep a CBT thought log of their anxious thoughts to review in each session.
9 – Couples Therapy Note Template and Example
Couples therapy notes are different than individual therapy notes as they focus on the dynamic between two people who are in relationship or marriage. Many couples come to therapy to work on improving their relationship through the work they do in couples therapy. An example of a couples psychotherapy note is outlined below.
Presenting Problem: The couple presents for therapy wanting to work on communication differences. The couple reports that when they try to communicate they often end up yelling at each other which results in no teamwork to accomplish their goals or solve problems. They state that they both end up shutting down which leads to an emotional disconnect. They state they want to work towards communicating better and finding ways to resolve conflict.
Themes and patterns identified: The social worker observed that the couple tends to sit far away from each other session. They appear physically and emotionally disconnected. The couple has insight into their challenges with ineffective communication, and report that the yelling and disrespectful communication increases when they are both stressed.
Discussion: The couple shuts down when they feel disrespected. They use stonewalling often to communicate a message, but this method drives them further apart as it doesn’t resolve the issue. The “silent treatment” then begins to feel like a punishment to them both, and they never talk about the issue again.
Plan: The social worker addressed and provided education to the couple about Gottman’s Four Horseman of the Apocalypse in session. The couple voiced understanding about what this means and were able to identify some examples of how this shows up in their relationship. The social worker will educate them on the antidotes to the four horsemen in the next session.
Homework: The couple was encouraged to write down any incidents of the four horseman appearing in their day to day life before the next session.
10 – PIE Note Template and Example for Mental Health Documentation
PIE notes are short progress notes that are problem-focused. Below is a PIE note example for adolescents, demonstrating the PIE notes model often used in clinical documentation for therapists.
Problem: The adolescent presents for a therapy session with reports of falling behind in school. The client reports that they have always been a straight A student, but their grades have worsened this year, which has been happening for about six months. They report an increase in the difficulty of their schoolwork. They say they have trouble focusing at school and home and avoid their homework because they find it challenging. The client states that when they are at school, the environment is “too loud to focus.”
Intervention: The counselor will work with the client on reducing the symptoms of ADHD. The counselor will work with the adolescent’s parents and school with permission from the client’s parents to request accommodations for the client at school. The counselor will educate the client on some strategies they can use to manage their ADHD. The counselor will also provide psychoeducation to the client and their parents on tools to help the client manage their ADHD.
Evaluation: The client’s symptoms are consistent with a diagnosis of ADHD. The client was receptive to this and the client and parents are on board for learning new strategies and working with the school.
11 – Play Therapy Note Template and Example
A play therapy notes follow various formats. It’s important to talk about how the child engaged in play therapy and what interventions you used. A play therapy note may follow a similar format as below.
Presenting problem: The child presents for therapy because the parents state the child throws more tantrums at home. The child is eight years old and in 2nd grade. The parents report the child is doing well in school but at home is refusing to clean their room and throwing tantrums when asked to do something. The parents say they want the child to learn to manage their emotions better.
Techniques: The Psychologist will provide client-centered play therapy techniques with the child to help the child work on better identifying and managing emotions. The Psychologist utilized tracking and limit setting during this session to help the client identify emotions.
Response: The child was shy and reluctant to engage in play therapy at first. The client then played with the dollhouse the majority of the session. The client preferred independent play, and shut down when the Psychologist talked about how the dolls might be feeling.
Plan: The Psychologist will continue to meet with the child weekly for play therapy. The Psychologist will continue to work towards building trust and rapport with the client.
Using automated therapy documentation or AI-generated progress notes for therapists can simplify record-keeping for child sessions.
12 – Group Therapy Note Template and Example
Group therapy notes are different than individual or couples therapy notes. They document what occurred in the group as a whole, and how the individual responded to the group facilitator and other members of the group. An example of a group therapy progress note for substance use is supplied below.
Group focus: The group focus today was identifying triggers to substance use. Identifying triggers for substance use is key in relapse prevention, and helps the group identify barriers to sobriety.
Client mood: The client presented with depressed mood.
Group facilitator interventions: The group facilitator encouraged the group to identify triggers that lead them to use drugs. The group facilitator encouraged sharing about their triggers to help them process what triggers they have. The group facilitator assisted the group members with identifying how the group members could respond to their triggers and make different choices or avoid their triggers altogether. The group members actively engaged in a discussion about avoidable and unavoidable triggers.
Individual response to group: The client responded well to the group discussion and was able to share about her triggers. She had to be prompted to engage at first, but then was an active participant in the group after some encouragement. ****
Plans and Recommendations: The group facilitator recommends that the client continue to attend group sessions on a weekly basis. The group facilitator also recommends that the client still attends individual therapy sessions weekly to address depression.
13 – Custom Format Therapy Progress Note Template and Example
Custom progress notes can be tailored for each individual clinician. They don’t have to follow these sections but here’s an example that includes a strengths section.
Presenting problem: The client presents for therapy, wanting to work on steps to come to terms with their sexuality. They report accepting parents but struggle with coming out to their extended family for fear of judgment. The client says they have moderate anxiety and would like some strategies for dealing with it.
Mental Status: The client presents with an anxious presentation. The therapist can sense that it is difficult for the client to attend therapy and discuss their sexuality.
Assessment: The client appears to have anxiety and seems nervous about discussing their sexuality in depth in the first session. The client will likely need to build trust and rapport with the therapist before digging into family history and coping.
Intervention: The therapist will educate the client on the stages of coming out. The therapist will first work to develop trust and rapport with the client. When the client is more trusting of the therapist, the therapist will use ACT techniques to help the client respond to coming out.
Strengths: The client can ask for help and has a strong support system consisting of friends and parents.
Areas to work on: The client is anxious and may have difficulty opening up initially.
Plan: The therapist and client will meet weekly.
14 – Mentalyc’s SOAP Note Example
This standardized note format meets the requirements for medical necessity and provides evidence-backed interventions, which make it easy to track client progress. Using Mentalyc progress note software is a leading solution for improving therapist productivity with templates.
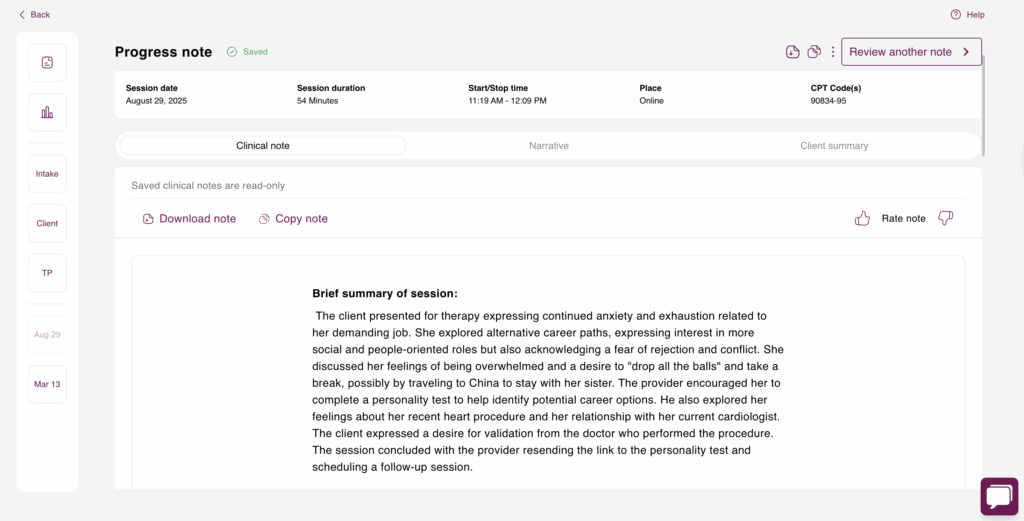
Subjective:
The client presented for therapy reporting fluctuating emotions, work stress, and self-critical thoughts, though she denied any self-harm. She described two instances of near emotional shutdown during the week. A review of her DBT diary card indicated moderate avoidance urges and distress (7/10) specifically related to a workplace conflict. The client’s work stress appears to be significantly impacting her emotional regulation and ability to manage conflict.
Objective:
The client’s presentation and concerns were assessed through a clinical interview and review of her DBT diary card. The diary card provided data on urges, skills utilization, and distress levels. Paced breathing and grounding techniques were utilized during the session. CBT work focused on restructuring the automatic thought, “I can’t handle this job, ” using Socratic questioning to generate counter-evidence. This led to the reframed thought, “The job is demanding, but I have evidence that I can manage it, ” with the client reporting a 65% belief in the new thought, up from 30%. Mindfulness practice was employed to help the client label her emotions (hurt, anxious, small) after she became tearful mid-session while recalling her supervisor’s tone, which triggered memories of childhood criticism. This intervention successfully reduced her distress level from 7/10 to 4/10. The session also explored the connection between her self-criticism, authority-triggered anxiety, and the core belief “I’m not good enough.”
Assessment:
The client actively engaged in the session and demonstrated a strong therapeutic alliance by openly sharing vulnerable emotions and experiences. She showed a positive response to both CBT and DBT interventions, successfully utilizing learned skills and demonstrating improved emotional regulation through mindfulness and thought reframing. While she presented with mild risk due to reported near emotional shutdown, her active engagement and willingness to utilize coping skills suggest a positive trajectory. Continued monitoring of her emotional distress remains important.
Plan:
The client’s homework includes daily paced breathing practice, particularly during work breaks; identifying and reframing automatic thoughts at least once per day; and continued use of the DBT diary card. Future sessions will focus on continuing CBT and DBT skill development to address work stress, self-criticism, and emotional regulation. Further exploration of the connection between current experiences and childhood experiences with a critical parent will be a focus of ongoing treatment.
Mentalyc AI Pricing Plans
| Plan | Price | Key Features |
| 14-Day Free Trial | $0 | 14 days of full PROaccess, including 15notes—no credit cardrequired. |
| Mini | USD 14.99 /month | Record in-personsessions, upload audiofiles, use voice-to-text,or type notes directly, etc |
| Basic | USD 29.99 /month | Everything in Mini, plus:Alliance Genie™ NEW!(limited access), Smart TP™ |
| Pro | USD 59.99 /month | EMDR, Play andPsychiatry modalities,100+ custom templatesincld. BIRP, PIRP,GIRP, PIE, and SIRP,Auto-computed CPTcodes |
| Super | USD 99.99 /month | Everything in Pro, plus: Group therapy notes foreach group member, Priority onboarding and support |
For more details, visit the pricing page.
15 – Example of a Mentalyc’s DAP Note
This AI-generated progress note for therapists succinctly summarizes the information the client shared during the session. It’s easy to read and clearly shows the client’s progress and the therapist’s actions. The example below demonstrates how to write therapy notes efficiently.
Data:
The client presented with significant anxiety (8/10) primarily related to work and health concerns, which consequently impacted her sleep and social interactions. She reported avoiding phone calls due to low energy. Her anxiety manifests as racing thoughts, difficulty sleeping, and avoidance of social interaction, significantly impacting her ability to connect with friends. The client’s current high anxiety levels have persisted over the past few days, escalating particularly at night.
Assessment:
Utilizing a clinical interview to assess the client’s anxiety, triggers, and treatment effectiveness, it was observed that the client actively engaged in the session and responded positively to the interventions. She demonstrated a willingness to practice coping skills and experienced a reduction in anxiety from 8/10 to 5/10 by the session’s end. She successfully formulated an alternative statement to challenge catastrophic thoughts and expressed motivation to continue practicing the discussed skills. However, the client also reported struggling with intrusive thoughts during mindfulness exercises, presenting a potential challenge to her continued practice. Due to her high anxiety and social withdrawal, she is considered to be at mild risk, necessitating continued monitoring.
Plan:
The client’s homework includes continuing mindfulness practice, particularly at night before bed. Furthermore, she is to practice reframing catastrophic thoughts when physical anxiety symptoms arise. She is also tasked with attempting one social connection, either by answering a call or initiating a brief check-in with a friend. Future sessions will focus on continuing work with CBT and DBT skills to manage anxiety and promote social engagement, as well as exploring any ongoing challenges with mindfulness practice. Continued weekly therapy sessions are planned to integrate CBT and DBT skills to manage anxiety, improve emotional regulation, and address avoidance behaviors.
Do you want to make progress notes easier?
If you want to streamline your note-taking and make writing progress notes easier, consider signing up for Mentalyc. Mentalyc’s AI technology can help you record your sessions and write notes so you have more time to focus on what matters to you. With an average of 2 minutes to write a progress note, this can save you time and headaches. Don’t hesitate; get started with Mentalyc today!
Still unsure? See what users are saying about Mentalyc:
Why other mental health professionals love Mentalyc

“My notes get finished after every single session now because Mentalyc makes it so easy. I’m not stressed out about notes and I feel like my notes are of much higher quality.”
Licensed Clinical Social Worker

“I go back and can read the notes, and it really helps me for the next session … it has made me a much better counselor.”
Licensed Professional Counselor

“It’s so quick and easy to do notes now … I used to stay late two hours to finish my notes. Now it’s a breeze.”
Licensed Professional Counselor

“For those who have hesitations … It is a lifesaver. It will change your life and you have more time to be present with your patients.”
Licensed Clinical Social Worker