Mastering SIRP Notes: Your Ultimate Guide to Crafting The Perfect Note (With Examples!)
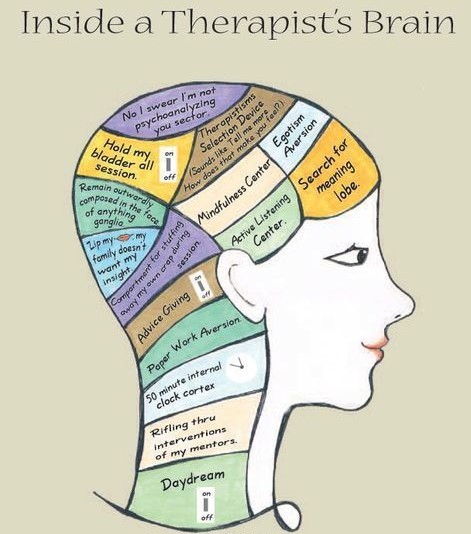
In the labyrinth of the mental health field, where our passion lies in healing minds, we often find ourselves entangled in the thorny embrace of administrative duties. Progress notes and documentation loom before us, demanding attention, and siphoning a significant portion of our professional lives. But fret not, for within the realm of these seemingly mundane tasks lies an art – a skill that can elevate your practice and bring order to the chaos.
As a therapist or mental health provider, you may be familiar with the ritual of crafting progress notes after each visit, an integral part of our journey as healers. Yet, beyond the surface-level obligation, these notes serve a grander purpose – one that weaves the fabric of comprehensive care, collaboration, and adherence to the highest standards of our profession.
While the BIRP and SOAP methods stand as two commonly employed templates for drafting progress notes, as we previously discussed in separate blogs, our focus today lies in exploring the intricacies of the SIRP template.
Journey with us as we unlock the secrets of SIRP notes and witness how our tips will empower your practice and elevate your clients’ experiences to unparalleled heights!

New! Transfer your notes to EHR with a single click. No more copy-pasting.
What Are SIRP Notes?
Short for “Situation, Intervention, Response, and Plan”,SIRP Notes provide a structured approach to help therapists better understand their clients’ emotional responses and reactions to specific situations.
The SIRP format represents one among the diverse array of available formats for drafting progress notes (SOAP, BIRP, PIRP, DAP, etc.), thereby ensuring meticulous adherence to all the requisites of the note. Moreover, this format serves as a valuable instrument for service providers, enabling them to utilize progress notes as an effective means of communication, yielding a comprehensive understanding of the rendered services and the status of the client.
Wanna Delve Deeper? Let’s Go!
S.I.R.P. serves as an acronym denoting four key components: Situation, Intervention, Response, and Plan.
Situation
This section demands a lucid and comprehensive depiction pertaining to the client’s prevailing complaints, conditions, and the assessment made during the session. Utilizing behavioral terminology, it is essential to include an evaluation of the client, avoiding diagnostic statements but rather elucidating the rationale behind the session.
This section encompasses an observance of the client’s overall presentation at the time of service, encompassing aspects such as personal hygiene, speech patterns, and mood, among others. It further necessitates a focus on any specific impairments. Additionally, it prompts an evaluation of the validity of the diagnosis, alongside an assessment of the progress achieved thus far.
As such one can perceive the situation section as revolving around the following:
- Notes of the client’s presentation at the time of service, e.g. hygiene, speech, mood, etc.
- Chief impairments and complaints.
- Diagnosis.
- Whether progress is being made.
Intervention
This section portrays the proactive measures undertaken by the staff (actions performed). Identify the skills employed to effectively manage, adapt, respond to, and solve the clients’ main complaints. Acknowledge the development of new behaviors and strengths. Specify the particular skills taught, demonstrated, and practiced. The intervention components within the progress note should encompass the following:
- Clinician’s interventions: Elucidate the actions undertaken by the clinician.
- Clinician’s assessment, encompassing a risk assessment if relevant.
- Document the advice and recommendations provided to the client and their family.
Response
In this section, make sure you depict the client’s response to your intervention; elucidate the response in terms of observable behavior while also evaluating the client’s progression or lack thereof. Furthermore, encompass a comprehensive assessment of the client’s overall response to treatment while delineating how the client received the intervention.
Therefore, the response section:
- Presents any novel discoveries/progress derived from the assessment process.
- Assesses whether there has been substantial progress or a notable absence of improvement – expound on the latter.
- Determines if the client comprehended and accepted the intervention or exhibited signs of resistance.
- Explicates the necessity for supplementary treatment based on medical requirements.
- Incorporates appropriate outcome measures within the documentation.
Plan
This segment encompasses a comprehensive delineation of clinical determinations pertaining to the individual seeking assistance, supplementary interactions with relevant parties, recommendations for external assistance and referrals, subsequent measures for ongoing engagement, tasks to be assigned for further progress, and sessions dedicated to the course of treatment. In instances where deemed suitable, this may encompass recommendations for accessing community resources and partnering with other organizations.
Furthermore, this section accommodates arrangements for any subsequent appointments.
As such, this section:
- Establishes the need for new goals and objectives.
- Substantiates the continued relevance of treatment objectives through documentation, or adapts them accordingly.
- In the event of inadequate progress, this section seeks to validate the diagnosis and/or make changes to existing objectives.
- Deliberates on treatment calibration and devises a plan for discharge.
SIRP Note Example (Sample)
First Name: John Last Name: Doe Date of Birth: 20/09/1990
Date/Time: 20/07/2023
Situation
John has been facing challenges with his anger problems in recent weeks, making it tough for him to interact with his family. He currently resides with his parents while searching for a job, but frequently loses his temper and admits, “I find it hard to control my actions when I get so furious.”
Intervention
John has received emotional regulation techniques to effectively handle his anger and cultivate a more positive outlook during challenging circumstances. We engaged in dialogue exercises to explore strategies for coping with life stressors, including his job search, which can intensify his feelings and trigger bouts of anger.
Response
John reacted favorably to the proposed plans, offering valuable insights and revelations concerning the negative thinking patterns during the conversational exercises. By employing emotional regulation techniques, he crafted effective strategies to identify the appropriate moments to disengage and defuse tense situations.
Plan
In two weeks’ time, John is scheduled to meet with me for a follow-up on his anger management progress. Should there be no noticeable improvements, we will then explore alternative methods of evaluation.
Clinician Name: Dr. Z Signature: S. Z.
Wanna Get It Done Perfectly?
Mastering the art of crafting impeccably composed progress notes constitutes an essential cornerstone in the repertoire of any proficient therapist. Within the tapestry of your professional endeavors, these well-crafted notes serve as a pivotal means to assess treatment efficacy, facilitating informed decisions regarding potential modifications to the therapeutic course.
Moreover, they serve as an invaluable navigational tool, steering therapeutic sessions purposefully, and warding off any meandering discourse devoid of pertinent elucidation.
The fallibility of human memory, when juxtaposed against the nuanced intricacies of interventions conducted in successive therapy sessions, renders reliance on remembering clients’ details an impractical endeavor.
Instead, availing oneself of the opportunity to peruse meticulously documented progress notes after each session bestows a profound advantage, reinvigorating the therapist’s cognizance of the client’s chief complaints, implemented treatment modalities, and predefined therapeutic objectives.
Indeed, the absence of such an organizational practice might beckon unforeseen consequences, encompassing not only professional ramifications but also legal and ethical quandaries.
It is therefore that we, at Mentalyc, share the following tips to guide your journey whilst ensuring you provide excellent care for your clients:
- Maintain a Professional and Concise Approach: Listen, one thing you have to recognize is that the progress notes you compile are liable to be perused by fellow healthcare professionals whenever your client seeks further consultation. As such, please refrain from excessive use of abbreviations that may confound other practitioners. This guarantees that anyone attending to the patient subsequently can readily glean a comprehensive overview of their medical history and prior treatment regimens.
- Adopt an Objective Narrative: Embrace the practice of drafting your notes in the third person, devoid of colloquialisms or personal sentiments regarding a client’s progress.
- Substantiate Observations with Unambiguous Evidence: Thoroughly substantiate your discernments by including clear indicators of a patient’s condition. For instance, if you denote a low mood, accompany it with explicit markers such as affect, body language, or the patient’s own accounts.
- Ensure Precision: Pay meticulous attention to the accuracy of pivotal information: dates, times, locations, and diagnostic codes. Though seemingly minor, these details hold paramount significance when reviewing notes and comprehending the patient’s progress over time.
- Play it Smart: The adoption of prepared templates can significantly enhance the organization of your note-taking process while saving time and energy, and guaranteeing the inclusion of all pertinent data. As you become acquainted with our ready-to-use templates, feel free to customize them to suit your preferences and devise a system that best complements your needs. Embrace Mentalyc’s presence resourcefully to optimize your practice.
Last But Not Least… Mentalyc Is Here!
As dedicated healthcare professionals, we understand the immense responsibility you carry, and it’s natural to feel overwhelmed when trying to decipher every detail from each session. Remember, you are only human, and even the strongest heroes sometimes can benefit from a little support.
You’re not alone in this. Embrace the practice of note-taking with confidence, knowing that it’s not just helpful but necessary. And should you ever feel unsure or need assistance, remember that Mentalyc is here to provide the support and guidance you need. You’ve got this, and we’re right behind you every step of the way!
References:
Sommers-Flanagan, J., & Sommers-Flanagan, R. (2017). Clinical Interviewing (6th ed.). John Wiley & Sons.
Juhnke, G. A., Granello, D. H., & Granello, P. F. (Eds.). (2016). Counseling and psychotherapy theories in context and practice: Skills, strategies, and techniques. John Wiley & Sons.
American Psychological Association. (2015). Guidelines for clinical supervision in health service psychology. American Psychologist, 70(1), 33-46. doi:10.1037/a0037896
Dillard, C. L., & Pinholster, A. S. (2018). The Psychotherapy Progress Note: A Descriptive Accountability Tool. Journal of Contemporary Psychotherapy, 48(1), 17-24. doi:10.1007/s10879-017-9374-3
Why other mental health professionals love Mentalyc

“It’s so quick and easy to do notes now … I used to stay late two hours to finish my notes. Now it’s a breeze.”
Licensed Professional Counselor

“By the end of the day, usually by the end of the session, I have my documentation done. I have a thorough, comprehensive note … It’s just saving me hours every week.”
CDCII

“It takes me less than 5 minutes to complete notes … it’s a huge time saver, a huge stress reliever.”
Licensed Marriage and Family Therapist

“A lot of my clients love the functionality where I can send them a summary of what we addressed during the session, and they find it very helpful and enlightening.”
Therapist