GIRP Notes
Most clinicians know the struggle of documentation that actually feel useful, not just like paperwork. GIRP notes were created with this in mind. Instead of getting lost in checkboxes or long narratives, GIRP progress notes guide you to start with a Goal what the client wants to work on. From there, you document the Intervention you used, the client’s Response, and the Plan moving forward. It’s a straightforward structure that mirrors the flow of a real session.
Because it’s easy to follow, GIRP documentation in therapy helps you stay focused on what matters most: the client’s progress. You can see at a glance where the work is heading, what’s been tried, and how the client is responding. Many therapists find that this style not only keeps their notes client-centered but also makes treatment planning and outcome tracking feel more natural and less burdensome.
GIRP Note Structure
| Section | Purpose | Example Content |
| Goals | Record the client’s short- and long-term objectives for therapy. | “Client wants to reduce anxiety during social situations.” |
| Intervention | Document what the therapist did to help the client move toward goals. | “Introduced breathing exercises to manage panic symptoms.” |
| Response | Capture how the client reacted to interventions and therapy process. | “Client reported feeling calmer after using the breathing technique.” |
| Plan | Outline the next steps for treatment and follow-up actions. | “Assign daily practice of breathing exercises; review progress next session.” |
How to write a GIRP note
GIRP progress notes have four distinct parts, with tailored information about the session in each part of the note.
Goals
The “G” in the GIRP note stands for goals. The goals section addresses what the client wants to work on in therapy.
The goals section includes information such as:
- Why the client is in therapy
- What they want to work on in therapy
- Why the client may need therapy
The Goals section is where you capture both short-term and long-term objectives. A helpful tip is to phrase these goals in the client’s own words whenever possible. By grounding this section in what the client truly wants from therapy, you not only clarify the focus of your work but also create meaningful therapy progress notes that directly reflect client needs. This makes the documentation more relevant, easier to connect to session content, and more useful when reviewing progress over time.
Intervention
The “I” in the GIRP note stands for intervention. The intervention section addresses what you, as the mental health professional, did.
The intervention section includes information such as:
- What interventions the therapist used
- How the therapist helped the client work towards achieving their goal
The intervention section may highlight the therapist’s theoretical orientation.
Response
The “R” in the GIRP note stands for the response. The response section focuses on how the client responds to the prescribed treatment.
The response section includes information such as:
- How the client is responding to therapy
- Client’s progress toward achieving their goals
- Their attitudes about therapy
- The therapist’s observations of client behavior, such as: Client has a flat affect, the client is withdrawn, etc.
The Response section is where you note how the client reacted to the interventions you used in session. This part should clearly show the reader of your clinical documentation how the client is progressing in therapy—whether they’re making gains, facing challenges, or showing mixed results. Responses can include emotional reactions, level of engagement, skill use, or changes in symptoms. Keeping this section specific and behavior-focused makes it easier to see patterns over time and provides a stronger foundation for treatment planning.
Plan
The “P” in the GIRP note stands for plan. The plan section discusses what happens next in the client’s therapy.
The plan section includes information such as:
- Referrals to other medical providers
- Topics of future sessions
- The date and time of the next session
- Any homework the therapist assigns to the client
The plan section discusses an actionable system for moving forward with the client’s treatment.
However, writing progress notes in the GIRP format can sometimes feel like extra work. The structure is clear and useful, but it also asks for a lot of detail—which can add to your documentation load. That’s where the Mentalyc Progress Note Generator comes in. Instead of spending valuable time typing out every section, you can generate GIRP notes in just a fraction of the time. The tool is designed for clinicians, with features that make it easy to create, edit, and manage progress notes while keeping them compliant and client-focused.
Example GIRP note for depression
If you need an example of what this may look like for a client with depression, here is an example:
Goals
The client met with the psychotherapist for an appointment on Tuesday at 1 p.m. The client reports they would like to learn three coping skills to help with depression. The client wants to implement these skills within the next month. The client also states in the long term; they would like to improve their mood and engage in activities they previously enjoyed, such as going to yoga class and spending more time with their friends. The client reports needing help because their low mood and lack of energy make it hard to engage in social relationships and hobbies they enjoy.
Intervention
The psychotherapist and client discussed the client’s depression during this session. The psychotherapist modeled a grounding exercise for the client during the session to help them cope with intense emotions when they feel overwhelmed. The psychotherapist taught the 5-4-3-2-1 grounding method, and the client voiced an understanding of how to use this skill. The psychotherapist and client also discussed obstacles to engaging in activities they used to like. The psychotherapist will focus on interventions for these obstacles in future sessions.
Response
The client responded well and appeared to understand the purpose of the 5-4-3-2-1 grounding exercise. The psychotherapist started with this exercise because the client reports that their symptoms of depression ramp up when they feel emotionally overwhelmed. The client was receptive to learning more coping skills and grounding practices in the future.
Plan
The psychotherapist will meet with the client again next Wednesday at 4 p.m. The client was assigned homework to implement the 5-4-3-2-1 grounding exercise before the next session if there are times when they are feeling emotionally overwhelmed. The client stated they wanted to talk to their doctor about depression medication and have a goal for themselves to call their primary care physician and schedule an appointment. The next session of the client will focus on learning more coping skills and grounding exercises.
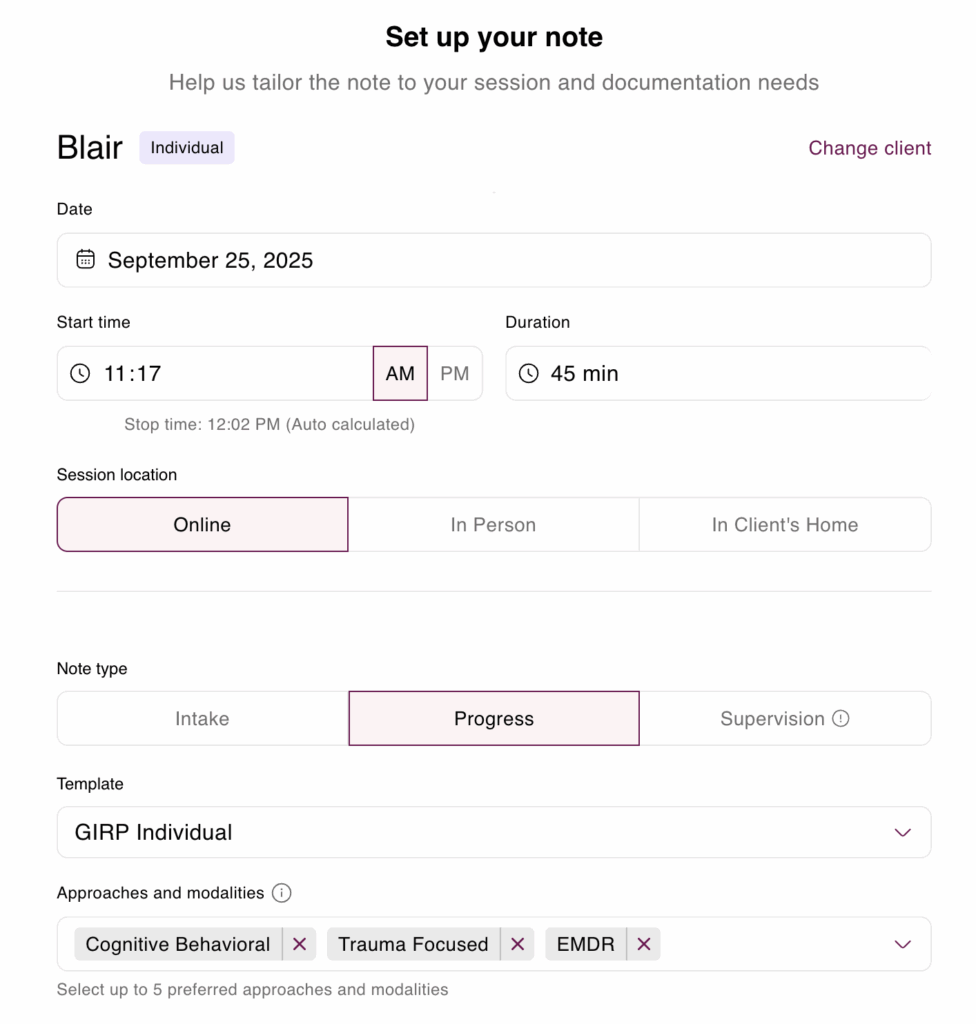
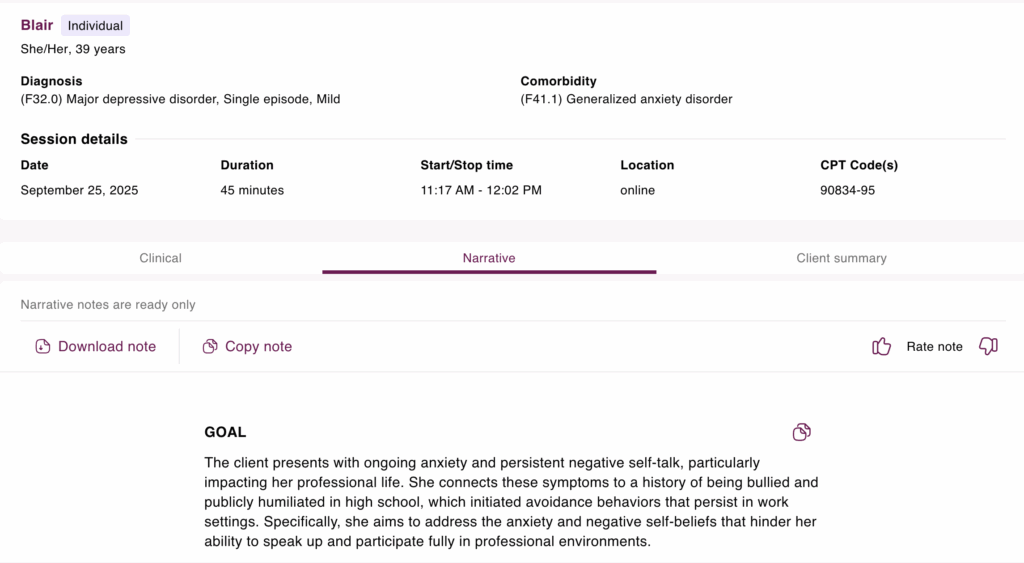
Mentalyc’s GIRP note example
Goal: The client presents with ongoing anxiety and persistent negative self-talk, particularly impacting her professional life. She connects these symptoms to a history of being bullied and publicly humiliated in high school, which initiated avoidance behaviors that persist in work settings. Specifically, she aims to address the anxiety and negative self-beliefs that hinder her ability to speak up and participate fully in professional environments.
Intervention: Building on previous CBT work, this session transitioned to a trauma-informed approach using EMDR. The client identified a core traumatic memory of being laughed at during a high school presentation, which triggers chest tightness and negative cognitions such as “I’m weak” and “Everyone sees I’m a failure. ” After psychoeducation on EMDR, the session focused on resource installation, guiding the client through a bilateral stimulation exercise to establish a ‘safe place. ‘ This intervention aimed to equip the client with a grounding resource before processing the targeted trauma.
Response: The client demonstrated positive engagement and insight, connecting her past trauma to current struggles. She actively participated in the EMDR resource installation and reported a reduction in anxiety and chest tightness following the exercise. Furthermore, she expressed hope that the therapy would help her gain control over the impact of past memories, indicating a shift in perspective and motivation for continued treatment.
Plan: For homework, the client will track daily triggers of anxiety, shame, and feelings of weakness, noting the specific situations and associated thoughts and feelings. This information will inform future EMDR processing. The next session will review this homework and begin gently processing the identified classroom memory, utilizing the established ‘safe place’ resource to manage potential distress. Continued treatment will employ EMDR to desensitize the client to the traumatic memory and facilitate the integration of more adaptive self-beliefs, such as “I am capable.”
Benefits of GIRP notes
Using the GIRP notes format offers various benefits. This note format is best when your client has clearly defined goals and objectives. When clients meet specific targets while working toward a larger goal, tracking their progress and reinforcing their ability to meet particular objectives is easy. This not only helps mental health professionals track client progress, but it helps the psychotherapist track client progress as well.
These goal-focused notes may also be beneficial for clinicians who are writing treatment plans. This style is easy to follow. Using the client’s stated goals and objectives for treatment planning is simple.
Comparison: GIRP vs SOAP vs DAP vs BIRP Notes
| Note Format | Sections | Primary Focus | Best Use Case |
| GIRP | Goals, Intervention, Response, Plan | Emphasizes goal-setting and tracking client progress | Ideal for goal-oriented therapy notes and documenting measurable outcomes |
| SOAP | Subjective, Objective, Assessment, Plan | Combines client reports, therapist observations, and clinical judgment | Best for clinical documentation for therapists with a diagnostic focus |
| DAP | Data, Assessment, Plan | Organizes client data and therapist assessment | Useful for concise mental health counseling notes |
| BIRP | Behavior, Intervention, Response, Plan | Highlights observed behavior and responses to treatment | Effective for therapist observation notes and behavior-focused therapy |
GIRP vs. SOAP Notes: Key Differences Explained
If you’re wondering if GIRP or SOAP notes are better, it’s a matter of personal preference. GIRP and SOAP notes both have four sections.
GIRP progress notes focus on goals, and SOAP notes focus on the subjective and objective aspects of a client’s behavior. GIRP progress notes also offer an intervention section and response section that focus on what the mental healthcare professional does in response to the client’s goals and responses to the interventions. In contrast, SOAP notes have an assessment section that focuses on the clinical judgments of the clinician.
Both GIRP and SOAP psychotherapy note formats have a plan section that helps the mental health professional document what’s next for the client’s treatment.
GIRP vs. DAP Notes: Which Is Best for Your Practice?
These are two formats if you’re trying to decide whether to use GIRP or DAP notes. But, again, your style of psychotherapy may determine what type of clinical documentation you like best.
GIRP progress notes focus on short and long-term client goals and the therapist’s interventions. In contrast, DAP notes focus on documentation of the client’s behavior and assessment of that behavior from the therapist. GIRP progress notes tend to be more client-oriented as your documentation reflects what the client wants from therapy, how you helped them progress toward their goals, and how they responded to your interventions. This makes GIRP an excellent choice for goal-oriented therapy notes.
Both GIRP notes and DAP notes—like many other formats—end with a Plan section. This step outlines what comes next for the client in therapy and is an essential part of clinical documentation for therapists. Having a clear plan not only supports continuity of care but also helps keep sessions focused and goal-directed.
GIRP vs. BIRP Notes: A Quick Comparison for Therapists
GIRP notes and BIRP notes are very similar documentation formats. Both documentation styles have four sections; the only differing section is the first. The GIRP note first section focuses on the client’s goals, which can include short and long-term goals and objectives. On the other hand, the first section of a BIRP note focuses on behavior rather than goals.
Both mental health note-taking styles have an intervention, response, and plan section. These sections discuss the therapist’s in-session interventions and the client’s response to treatment. Finally, both note styles outline the next steps for the client’s treatment.
With Mentalyc, you’re not locked into a one-size-fits-all format. You can choose from GIRP, SOAP, BIRP, DAP, and more – and even adjust the templates to best fit your needs and therapeutic modality. Mentalyc makes it simple to keep your documentation consistent, compliant, and aligned with the way you actually practice.
Quick Overview of A GIRP Progress Note
If you want an easy way to remember what goes into a GIRP note, consider using the guide below:
Goals
Some helpful tips for the goals section include:
- Using client quotes for what they state they want out of therapy
- Remember, it can be short or long-term goals
- Think about the client’s presenting problem to write the goals section
The goals section helps you track why the client is there and sets the frame for therapy.
Intervention
To make the intervention section easier and quicker to write, consider these tips:
- Record what the mental health professional does to help the client reach their goals
- Use an intervention words list to speed up this section
- Use interventions based on your style or way of doing therapy
The intervention section focuses on the role of the mental health counselor.
Response
If you’re finding the response section challenging, consider the following:
- Using Client quotes about what they find helpful and unhelpful
- Document what is and isn’t working for the client
- Record any feelings the client is having about the process of therapy
The response section helps you track your client’s progress and readjust the course of treatment if necessary.
Plan
When writing the plan section, consider these questions:
- Did I give the client homework?
- When is the date and time of our next session?
- Will the client follow up with any outside referrals?
- Did I send the client any resources to use outside of the session?
The plan section is always about the following action steps for you and the client to continue therapy.
From GIRP to BIRP, SOAP to PIRP and more, Mentalyc has you covered with customizable counseling documentation templates for every stage of care—from intake paperwork to treatment planning and ongoing progress notes. Instead of juggling different formats, you can keep everything consistent and client-centered in one place. With Mentalyc’s tailored solutions, it’s easier to streamline your workflow, stay compliant, and improve the quality of your mental health counseling notes without adding more to your plate.
✨ See how Mentalyc changed the way clinicians handle their notes:
Why other mental health professionals love Mentalyc

“My notes get finished after every single session now because Mentalyc makes it so easy. I’m not stressed out about notes and I feel like my notes are of much higher quality.”
Licensed Clinical Social Worker
“A lot of my clients love the functionality where I can send them a summary of what we addressed during the session, and they find it very helpful and enlightening.”
Therapist

“By the end of the day, usually by the end of the session, I have my documentation done. I have a thorough, comprehensive note … It’s just saving me hours every week.”
CDCII

“It immediately changed my quality of life, personally and professionally.”
Owner/Independently Licensed Marriage & Family Therapist (LMFT)
Mentalyc Plans & Pricing
| Plan | Price | Key Features |
| 14-Day Free Trial | $0 | 14 days of full PROaccess, including 15notes—no credit cardrequired. |
| Mini | USD 14.99 /month | Record in-personsessions, upload audio files, use voice-to-text, or type notes directly, etc |
| Basic | USD 29.99 /month | Everything in Mini, plus: AllianceGenie™NEW! (limitedaccess), Smart TP™ |
| Pro | USD 59.99 /month | EMDR, Play andPsychiatry modalities,100+ customtemplatesincld. BIRP, PIRP,GIRP, PIE, and SIRP,Auto-computed CPTcodes |
| Super | USD 99.99 /month | Everything in Pro,plus: Group therapynotes for each groupmember, Priorityonboarding andsupport |
For more information, visit the pricing page on our website.