Cognitive Behavioral Therapy (CBT) is one of the most commonly-employed and validated forms of psychotherapy, which helps individuals recognize their distorted thinking processes and bridge those distortions with corresponding behaviors. The primary concept is that our thoughts, emotions and actions are all connected with each other in a way so if we change one of them it can have positive effect on others as well.
Download the CBT Cheat Sheet (PDF)
Get the full printable version of this cheat sheet to use in your clinical work.
Download PDF ↓CBT was developed in the 1960s by Dr. Aaron Beck, who noticed that his patients often had internal dialogues that affected their emotions and behaviors. He found that by helping patients identify and challenge these thoughts, they could improve their mental health.
The therapy typically involves:
- Identifying problematic thoughts and beliefs
- Challenging these thoughts and beliefs
- Replacing them with more realistic and positive ones
- Changing behaviors based on these new thought patterns
CBT is structured and goal-oriented, often involving homework assignments between sessions. It’s typically short-term, focusing on current problems rather than past experiences, though it may explore how past events influence present thinking.
CBT is effective for a wide range of mental health issues, including:
- Depression
- Anxiety disorders
- Phobias
- PTSD
- OCD
- Eating disorders
- Substance abuse
- Sleep disorders
One of CBT’s strengths is its adaptability. It can be delivered in various formats, including individual therapy, group sessions, online platforms, and self-help books. This flexibility makes it accessible to many people.
Documenting that work, however, can be time-consuming. That’s why many clinicians use Mentalyc, which turns CBT session recordings into clear progress notes and generates a treatment plan in seconds, suggesting practical goals and measurable objectives that fit your client.
CBT equips individuals with practical skills to manage their mental health long-term. Patients learn to:
- Recognize distortions in their thinking
- Reevaluate their thoughts in light of reality
- Understand others’ behavior and motivations
- Develop problem-solving skills
- Build self-confidence
Core Beliefs and Principles of Cognitive Behavioral Therapy (CBT):
- Cognitive Model: A fundamental belief that our emotions and behaviors are influenced by our thoughts. This model suggests that it is not the events themselves but how we interpret them that cause our reactions.
- Collaborative Empiricism: The therapist and client become a unit working together to identify, evaluate, and respond to thoughts and beliefs. Active involvement from both parties is emphasized in this approach.
- Here-and-Now Focus: CBT recognizes past experiences but mainly deals with immediate thoughts and behaviors relevant to the client’s life now.
- Time-Limited and Goal-Oriented: In CBT, there are typically short-term interventions with specific goals set at the start of therapy.
- Structured Sessions: Typically each session has a particular agenda and structure which often includes review of homework assignments as well as setting new ones.
- Psychoeducation: Clients can learn about their diagnosis and what they need to do using the CBT model so that they can take control over themselves like therapists do.
- Cognitive Restructuring: This involves recognizing maladaptive thoughts, questioning them, and then changing them into healthy thought patterns.
- Behavioral Activation: Behavioural activation means encouraging patients to participate in activities which could make them feel better or challenge negative thinking patterns.
- Exposure Therapy: It entails gradually exposing oneself to feared situations or stimuli under controlled conditions for alleviating anxiety, avoiding panic attacks.
A treatment plan is a structured, comprehensive document that outlines the therapeutic strategy for addressing a client’s mental health concerns. It serves as a roadmap for therapy, guiding both the therapist and client throughout the treatment process.
Key components of a CBT treatment plan typically include:
- Presenting Problem: A clear description of the client’s primary issues and reasons for seeking therapy.
- Diagnosis: If applicable, the formal mental health diagnosis based on standardized criteria.
- Goals: Specific, measurable objectives that the client aims to achieve through therapy.
- Interventions: The therapeutic techniques and strategies that will be used to address the client’s issues and achieve the set goals.
- Timeline: An estimated duration for treatment and frequency of sessions.
- Progress Indicators: Measurable markers that indicate improvement or goal achievement.
- Resources: Additional support systems or resources that may be utilized during treatment.
- Potential Obstacles: Anticipated challenges and strategies to overcome them.
- Collaboration: Details on how the therapist and client will work together.
- Review and Revision: Plans for periodic assessment and adjustment of the treatment plan as needed.
A well-crafted treatment plan ensures that therapy is focused, efficient, and tailored to the individual client’s needs.
CBT Treatment Aim:
The primary aim of Cognitive Behavioral Therapy (CBT) is to help clients identify and change negative or distorted thinking patterns and behaviors that contribute to their psychological distress. Specific aims include:
Symptom reduction: Alleviating symptoms of mental health disorders like depression, anxiety, or PTSD.
Skill development: Teaching clients coping strategies and problem-solving skills.
Cognitive restructuring: Helping clients recognize and modify unhelpful thought patterns.
Behavioral change: Encouraging healthier behaviors and reducing maladaptive ones.
Relapse prevention: Equipping clients with tools to maintain improvements and handle future challenges.
Let us make use of examples for you to understand how a treatment plan using CBT can look like –
Common CBT Treatment Plan:
Assessment Phase (1-2 sessions):
- Conduct a comprehensive intake interview
- Administer relevant psychometric tests
- Identify presenting problems and set initial goals
- Provide psychoeducation about CBT
Treatment Phase (8-16 sessions):
a. Cognitive Restructuring:
- Identify negative automatic thoughts
- Challenge and reframe distorted thinking patterns
- Develop more balanced and realistic thoughts
b. Behavioral Activation:
- Increase engagement in pleasurable activities
- Set and achieve small, manageable goals
- Gradually increase activity levels
c. Problem-Solving Skills:
- Teach structured problem-solving techniques
- Practice applying these skills to real-life situations
d. Relaxation Techniques:
- Introduce and practice deep breathing exercises
- Teach progressive muscle relaxation
- Explore mindfulness techniques
e. Exposure Therapy (if applicable):
- Create a hierarchy of feared situations
- Gradually expose client to feared stimuli
- Process the experience and challenge associated beliefs
Maintenance and Relapse Prevention (2-4 sessions):
- Review progress and achievements
- Identify potential future challenges
- Develop a relapse prevention plan
- Schedule booster sessions if necessary
CPT Treatment Plan for Social Anxiety Disorder:
Client: Sarah, 28-year-old female
Diagnosis: Social Anxiety Disorder (SAD)
Duration: 16 weekly sessions
Goals:
- Reduce anxiety in social situations by 50% (measured by SPIN)
- Increase participation in social activities from 1 to 3 times per week
- Improve assertiveness skills in work meetings
Intervention:
Cognitive Restructuring (Sessions 1-4):
- Identify and challenge negative automatic thoughts about social situations
- Develop more balanced, realistic thoughts
Exposure Therapy (Sessions 5-12):
- Create hierarchy of feared social situations
- Gradually expose client to situations, starting with least anxiety-provoking
- Process experiences and challenge associated beliefs
Social Skills Training (Sessions 13-14):
- Practice assertiveness techniques
- Role-play challenging social scenarios
Relapse Prevention (Sessions 15-16):
- Develop coping strategies for future social challenges
- Create a maintenance plan
CBT Treatment Plan for Major Depressive Disorder:
Client: John, 45-year-old male
Diagnosis: Major Depressive Disorder (MDD)
Duration: 20 weekly sessions
Goals:
- Reduce depressive symptoms by 60% (measured by BDI-II)
- Increase daily activities from 2 to 5
- Improve sleep quality (7 hours of uninterrupted sleep)
Intervention:
Behavioral Activation (Sessions 1-6):
- Schedule and engage in pleasurable activities
- Gradually increase activity levels
Cognitive Restructuring (Sessions 7-14):
- Identify and challenge depressive thoughts
- Address negative core beliefs
Sleep Hygiene (Sessions 15-16):
- Implement sleep hygiene techniques
- Address nighttime rumination
Problem-Solving Skills (Sessions 17-18):
- Teach and practice problem-solving techniques
Relapse Prevention (Sessions 19-20):
- Identify early warning signs of depression
- Develop a relapse prevention plan
CBT Treatment Plan for Generalized Anxiety Disorder:
Client: Emily, 35-year-old female
Diagnosis: Generalized Anxiety Disorder (GAD)
Duration: 14 weekly sessions
Goals:
- Reduce overall anxiety by 50% (measured by GAD-7)
- Decrease daily worry time from 3 hours to 30 minutes
- Improve sleep onset latency from 1 hour to 20 minutes
Interventions:
Psychoeducation and Relaxation Training (Sessions 1-2):
- Educate about GAD and anxiety cycle
- Teach and practice deep breathing and progressive muscle relaxation
Cognitive Restructuring (Sessions 3-6):
- Identify and challenge worry thoughts
- Develop more balanced, realistic thoughts
Worry Management Techniques (Sessions 7-10):
- Implement worry scheduling
- Practice worry postponement
- Distinguish between productive and unproductive worry
Problem-Solving Training (Sessions 11-12):
- Teach structured problem-solving for real-life stressors
Relapse Prevention (Sessions 13-14):
- Review and consolidate learned skills
- Develop a personalized anxiety management plan
CBT Treatment Plan for Anxiety:
Assessment Phase (1-2 sessions):
- Conduct a comprehensive intake interview
- Administer anxiety scales (e.g., Beck Anxiety Inventory)
- Identify specific anxiety triggers and avoidance behaviors
- Provide psychoeducation about anxiety and CBT
Treatment Phase (12-16 sessions):
a. Cognitive Restructuring:
- Identify anxiety-provoking thoughts
- Challenge cognitive distortions (e.g., catastrophizing, fortune-telling)
- Develop more balanced and realistic thoughts
- Address core beliefs related to anxiety
b. Exposure Therapy:
- Create a hierarchy of feared situations
- Gradually expose client to anxiety-provoking stimuli
- Process the experience and challenge associated beliefs
- Practice in vivo exposure when appropriate
c. Relaxation Techniques:
- Teach diaphragmatic breathing
- Practice progressive muscle relaxation
- Introduce mindfulness meditation
d. Behavioral Experiments:
- Design experiments to test anxiety-related beliefs
- Conduct experiments and evaluate outcomes
- Use results to modify beliefs and behaviors
e. Worry Management:
- Identify productive vs. unproductive worry
- Implement worry scheduling techniques
- Practice worry postponement
f. Interoceptive Exposure (for panic disorder):
- Induce physical sensations associated with panic
- Challenge misinterpretations of bodily sensations
- Reduce fear of physical symptoms
g. Problem-Solving Skills:
- Teach structured problem-solving techniques
- Apply these skills to anxiety-provoking situations
Maintenance and Relapse Prevention (2-4 sessions):
- Review progress and achievements
- Identify early warning signs of anxiety relapse
- Develop a relapse prevention plan
- Schedule booster sessions if necessary
Bonus CBT worksheets that you can use with your clients :
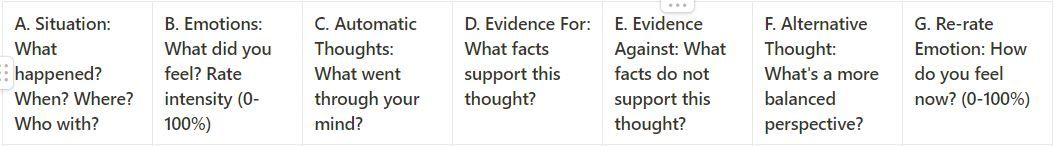
Worksheet 1
This is one of the most basic and widely used CBT tools. It helps individuals identify and challenge negative thought patterns.
Instructions:
- Describe the situation that led to your unpleasant emotion.
- Record your emotional reaction and rate its intensity.
- Write down the automatic thoughts that occurred.
- List evidence that supports and doesn’t support your thought.
- Create a more balanced alternative thought.
- Re-rate the intensity of your emotion.
- Behavioral Activation Schedule
Worksheet 2
This worksheet is designed as a weekly planner to help increase engagement in positive activities, particularly useful for individuals dealing with depression.
Instructions:
- Plan activities for each part of your day throughout the week.
- Focus on tasks that may bring a sense of pleasure or achievement.
- After completing each activity, rate it for pleasure and achievement on a scale of 0-10.
- At the end of the week, review your ratings to identify which activities brought the most pleasure or sense of achievement.
- Use this information to plan more enjoyable and fulfilling activities in future weeks.
Conclusion
In conclusion, you can keep the following points in mind when devising a treatment plan using CBT.
- Individualization
- Collaboration with client
- Measurable goals
- Flexibility
- Evidence-based interventions
- Skill-building focus
- Regular review and adjustment
- Cultural sensitivity
- Homework integration
- Relapse prevention strategies
In developing a plan of treatment in CBT, it has to be individualistic, collaborative, goal-oriented, and yet flexible. It is important to make use of empirically validated techniques and emphasize building skills with regular reviews. Additionally, cultural sensitivity, homework, and relapse prevention planning have to be provided for comprehensive care. By following these tenets, therapists can come up with an efficacious treatment plan that is client-centered and can effect positive change in the client, leaving them with equally valuable tools to self-manage their mental health outside the therapy setting.
Disclaimer
All examples of mental health documentation are fictional and for informational purposes only.
Why other mental health professionals love Mentalyc

“Do yourself a favor, make your life easier. I found Mentalyc to be one of the best tools that I’ve ever used.”
Licensed Marriage and Family Therapist

“For anyone hesitant: this is a lifesaver. It will change your life, and you have more time to be present with your patients.”
Licensed Clinical Social Worker

“It immediately changed my quality of life, personally and professionally.”
Owner/Independently Licensed Marriage & Family Therapist (LMFT)

“If I were recommending this software to a colleague, I would tell them that it is the best thing that they could do for their practice.”
Licensed Professional Counselor







